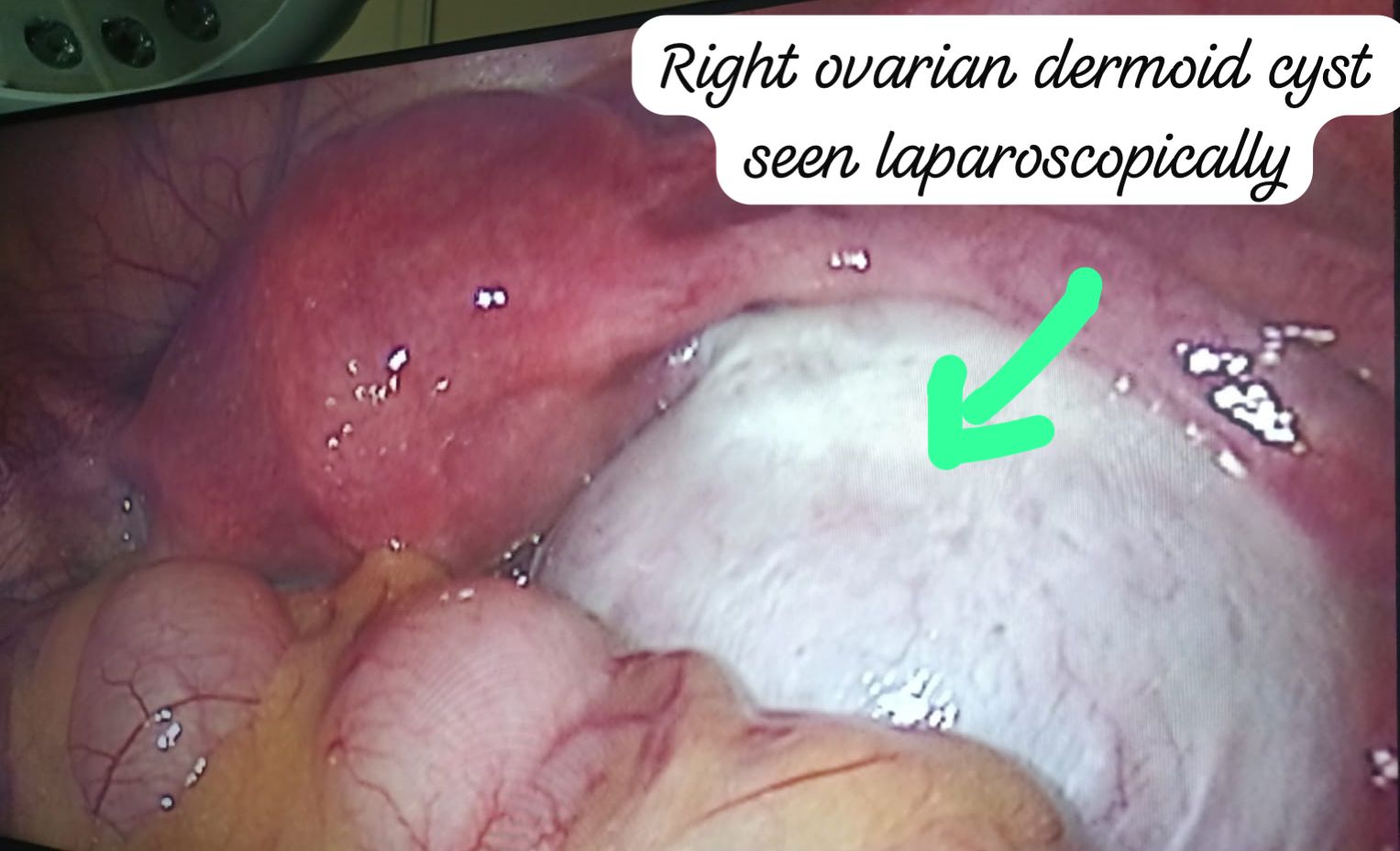
Ovarian Dermoid Cyst
An ovarian dermoid cyst is a benign growth that contains fully developed tissue such as skin, hair, teeth, or even nerve tissue. Unlike typical ovarian cysts that develop during the menstrual cycle, dermoid cysts are congenital and result from cells that form abnormally before birth. Though non-cancerous, these cysts can cause complications if they grow large or twist the ovary.
Who is affected by ovarian dermoid cysts?
Anyone with ovaries can develop an ovarian dermoid cyst. They are usually present from birth but may not be discovered until adulthood during imaging tests or pregnancy evaluations. These cysts are among the most common benign ovarian germ cell tumors and are often found incidentally.
How common are ovarian dermoid cysts?
Dermoid cysts are the most frequent type of benign ovarian tumor, accounting for nearly one-third of all benign ovarian masses found during pregnancy. In about 10–15% of cases, they appear in both ovaries.
How do ovarian dermoid cysts affect the body?
While usually harmless, complications may arise if the cyst grows large or causes ovarian torsion or rupture. These include:
- Ovarian torsion: Large cysts can twist the ovary, cutting off blood supply and causing severe pain or tissue death.
- Rupture: If the cyst bursts, it can release contents into the abdomen, sometimes leading to infection or inflammation requiring emergency care.
In rare cases (less than 2%), dermoid cysts may become cancerous, especially in women over 45 or when the cyst grows rapidly beyond 10 cm.
Symptoms
Most dermoid cysts are asymptomatic unless large. When symptoms occur, they may include:
- Abdominal pain or pressure
- Bloating or fullness
- Nausea and vomiting
- Constipation or appetite changes
- Pain during intercourse (dyspareunia)
Causes
Ovarian dermoid cysts form due to abnormal growth of embryonic cells that were meant to develop into other tissues such as skin, hair, or teeth. Over time, these tissues accumulate, forming a benign mass within the ovary. The presence of sweat glands within the cyst can lead to the secretion of oily substances (sebum), contributing to cyst growth.
Diagnosis
Since dermoid cysts often cause no symptoms, they are typically discovered during imaging such as an abdominal or transvaginal ultrasound. They have a distinctive appearance that makes them easily identifiable. Occasionally, an MRI is used to gain more insight into their composition.
Management and Treatment
Not all ovarian dermoid cysts require removal. Your doctor may recommend surgery if the cyst is large (over 5 cm), symptomatic, or has a risk of becoming malignant.
- Ovarian cystectomy: Only the cyst is removed, preserving the ovary and fertility.
- Oophorectomy: The entire ovary with the cyst is removed if necessary.
Most procedures are performed via laparoscopy (keyhole surgery), which uses small incisions for quicker recovery and minimal scarring.
Do dermoid cysts recur after removal?
Surgical removal is typically curative. Recurrence occurs in only about 3–4% of cases, making laparoscopy a safe and effective treatment option.